Female Pelvic Health; Week 1
From Pavement to Pelvis: Understanding Prolapse and your Runner’s Body
This Newsletter is about you understanding YOUR body. To help you identify if you have signs that a prolapse check might be beneficial.
We will dive into more info on what that looks like:
We will cover:
- Prolapse statistics in runners – does anyone else suffer too?
- What to look out for as a runner – is prolapse a current or future barrier to you?
- Why it happens to runners – what is going on with your body
- Tips for runners – Things you can do straight away to help
- What support is available? -You don’t have to run with it

Statistics:
The problem…
- only 12-13% of runners report pelvic organ prolapse
However prolapse is hard to quantify due to difficulty in diagnosis and linking symptoms to prolapse.
- On questioning 59% of elite athletes report some symptoms of pelvic floor dysfunction (PFD).
- Athletes with PFD report frustration and reduced concentration during performance.
- Fewer than 30% of athletes are aware of pelvic floor health.
- 88% have not undergone screening.
- Most do not disclose symptoms (78.2%)
- 95.1% do not seek specialised care.
Why live with it? Why train with it? Why run with it? Why compete with it?
#addressyourbarriersnow
#yourbodyyourjourney

I am a runner…What should I look out for?
A prolapse is where one of your three pelvic organs, (bladder, womb or bowel) can slip down into a lower position. This new resting position can cause symptoms and can be constant or come and go (intermittent).
You may benefit from a physio pelvic health check up if you notice any of the following…
✔ Heavy, dragging or weighted feeling in the vagina
✔ Sensation of a bulge, a lump or something feeling like it might fall out.
✔ Feeling discomfort “down there”
✔ Fatigue and aching between the legs
✔ Feeling like a tampon is stuck
✔ Soreness, aching in the lower abdomen or back
✔ Feeling like your bladder is not empty when you have been to use the toilet
✔ Feeling like you cannot empty your bowel fully
Remember symptoms can be during a run, towards the end of a run, or after a run.
Depending on the nature of the prolapse you may find:
- Symptoms improve when:
- Lying down
- After rest or overnight
- Symptoms worsen with:
- Long runs
- High mileage weeks
- Faster pace or interval training
- Running late in the menstrual cycle or when fatigued
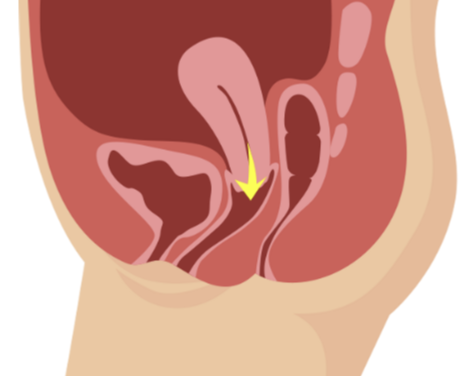
Picture of prolapse:
A prolapse can be any one or more of your organs (bladder, bowel or womb) slipping down into a lower position.
Approx 50% of women will have some degree of pelvic organ prolapse.

Why do runners get prolapse symptoms?
Running is a high-impact activity. Each foot strike generates forces in the pelvis equivalent to approximately 2.4–3.9× body weight, increasing intra-abdominal pressure (IAP) and loading the pelvic floor with every stride.
- Intra-abdominal pressure (IAP) rises with running speed, creating repeated downward forces on pelvic support structures.
- If pelvic floor muscles are weak, poorly coordinated or fatigued, they may not effectively counteract these pressures.
- Running also causes transient changes in pelvic floor tissue support immediately after a run. (This means the muscles that act as a sling underneath and around your organs, become lengthened and increase in size following a run). This is not an issue in healthy runners, but with those that are already compromised, this subtle change can be enough to cause symptoms.
- With prolapse, tissues that already have reduced support are stressed further by repetitive loading, potentially increasing symptoms of bulge, heaviness, pressure or urinary/bowel leakage.
Correct breathing, coordinated pelvic floor function and core stability all play a role in how the body handles these loads. Keep reading for more information…

Tips
Footwear – try to wear supportive footwear to ensure running technique is optimised, compensations are reduced, and impact is minimised.
Hydration – try to keep hydrated and avoid limiting your drinks. Dry tissues can feel more sensitive and irritated than healthy tissues. Especially the tissues around the vulva and inside the vagina.
Tune in – listen to your body. If you are worried your running is causing a problem make a note of when this happens, is it at a certain distance? When your breathing changes? When your effort increases? Or is it related to the time in your cycle? All of these things can be helped with specialist input (see below) and it is not something that you should have to modify to continue in the long term.
Stay active – do not panic exercise is good for us. Working with a health professional you can keep as active as possible whilst having the confidence that you are not making anything worse. In the meantime exercise in your asymptomatic range, keep going and seek support to help you build to where you want to be.
For more information on what can be done to help, including gadgets, see below
Further support…
So the good news is that pelvic health physiotherapy is highly effective.
Physiotherapy can improve prolapse by up to a stage, it can significantly improve bladder, bowel and vaginal symptoms and can reduce the length of gap in the levator (pelvic floor muscles) which support the organs.
It is a first line treatment for pelvic organ prolapse, it is cost effective and recommended by NICE guidelines and A level Evidence.
Significant results are usually seen within 16 weeks of starting a supervised training programme.
What does pelvic health physio involve for female runners with prolapse issues?
✔ Functional Pelvic floor assessment and treatment (e.g. standing dynamic assessment)
✔ Evidence, experience and national guideline based pathway
✔ Use of a vaginal pessary (where appropriate) to alleviate symptoms
✔ Strength AND timing (pelvic floor, trunk, leg)
✔ Relaxation
✔ Impact control
✔ Running-specific rehab
✔Referral on if required
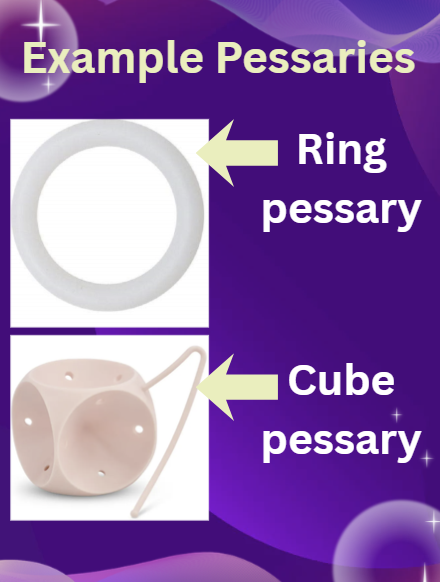
Vaginal Pessaries
There are various pessaries that can be worn during running to manage prolapse symptoms.
They come in many different sizes, to match the many different shapes of vagina’s.
These are soft, comfortable devices that can be used for each run, or left in place for a period of a few months. This reduces movement of the vaginal walls during running to reduce or even STOP symptoms.
Below are a few examples of devices available which can be fitted by specialist female pelvic health physio (alongside specialist pelvic health input).
See the statistics for Pessaries below…

For further support, an individual assessment and management plan to stop prolapse issues interfering with running, book an initial pelvic health appointment.
Alternatively you can book a FREE video or telephone consultation with Jodie to find out if we can help.
References:
- Prevalence of pelvic floor dysfunction in recreational athletes: a cross-sectional survey – PMC
- Nearly half of 325 athletes reported pelvic floor symptoms: a cross-sectional study at the Lima 2024 World Athletics U20 Championships | BMJ Open Sport & Exercise Medicine
- Do women runners report more pelvic floor symptoms than women in CrossFit®? A cross-sectional survey – PubMed
- Overview | Urinary incontinence and pelvic organ prolapse in women: management | Guidance | NICE
- Effect of pelvic floor muscle training on pelvic floor muscle morphometry in subjects with pelvic organ prolapse: a systematic review and meta-analysis – PubMed
WANT MORE INFO:
Book in for a free 10 min consult with JODIE
Or book an initial Pelvic Health physiotherapy appointment with JODIE
Spread the word, empower yourself and others…

Jodie our clinical lead in Pelvic Health brings 18 years of experience of improving the lives of women living with sensitive issues such as pain, prolapse, urinary leakage, bowel leakage and sexual dysfunction. Her experience comes from working as a Clinical Specialist in Female Pelvic Health in the NHS and as clinical educator to Midwives, GP’s, Physiotherapists, Consultants and Registrars in all aspects of pelvic health.
You can book a FEMALE PELVIC HEALTH appointment with JODIE HERE

