‘Why do I feel uncomfortable down there’
This week’s newsletter focuses on Prolapse.
We will cover:
- What a prolapse is
- Main symptoms of prolapse
- Main risk factors for developing a prolapse
- What we can do to prevent a prolapse, or prevent worsening if we have one

So grab your favourite (decaff) drink and read on…
It is never too early to understand and prevent!
& if you think you may have symptoms ACT NOW
Invest in your best asset: You
Don’t forget to share with your friends and family too, educate your partners and sons. Help them to understand and support you and your wider family.
Diagram of a healthy pelvis:
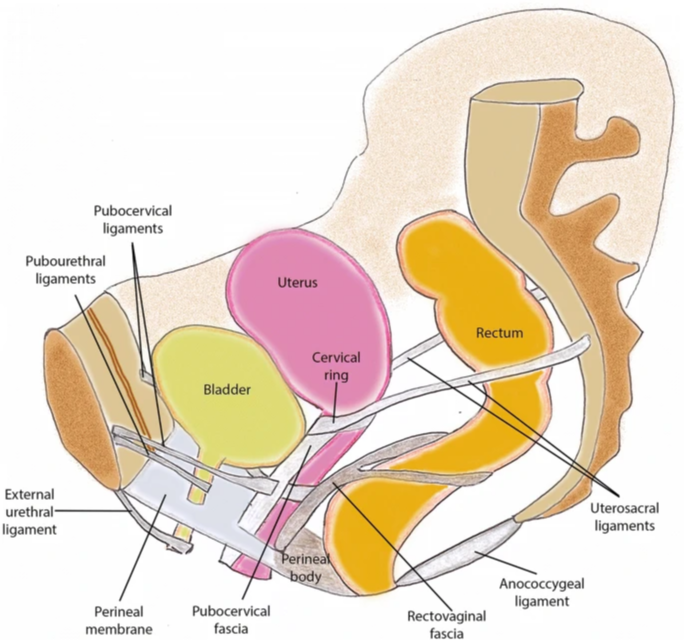
What is a prolapse?
A prolapse is where one or more of the organs within the pelvis (bladder, womb or bowel) can drop down lower into the pelvis and bulge into the vagina.
A prolapse is not life threatening, but it can cause worry, pain and discomfort. Many women stop doing activities and exercise, however with assessment and support from a professional, most activities are safe to continue with.*
*This will depend what is prolapsing, the stage of the prolapse and the activity in question. See a health professional for more information. You can book a pelvic health appointment with Jodie or if you would like to discuss if you would benefit from an appointment you can book a FREE 10 minute telephone or video consultation.
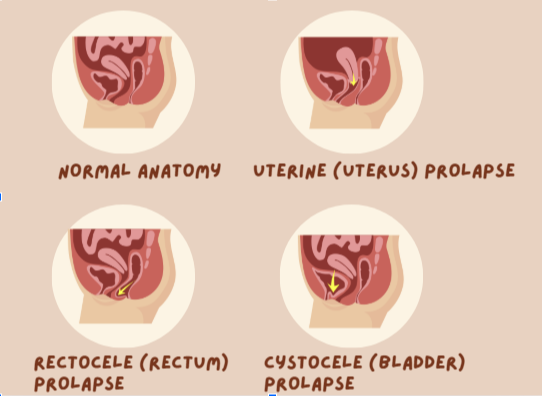
Common symptoms of pelvic organ prolapse:
- A feeling of heaviness around your lower stomach and / or vagina
- A dragging discomfort inside your vagina
- A feeling like there’s something coming down into your vagina – (or feeling like you have a tampon stuck)
- Feeling or seeing a bulge in or outside of your vagina
- Discomfort or change to sensation during sex
- Changes to your bladder – such as feeling like your bladder is not emptying fully, needing to go to the toilet more often, or leaking a small amount of pee when you cough, sneeze or exercise (stress incontinence)
- Changes to your bowel – difficulty starting, or finishing a bowel movement. Feeling like your bowel motion is getting stuck.
Sometimes pelvic organ prolapse has no symptoms and is found during an internal examination carried out for another reason, such as a smear test.
Most symptoms can usually be improved with physiotherapy which may include pelvic floor exercises and lifestyle changes. Keep reading below to see what physiotherapy can do to help.
Let’s look at the Statistics:
– Up to 50% of women may have some degree of prolapse on examination, (not all are symptomatic).
– Despite the number of women living with prolapse, 53% of women with symptoms don’t seek help.
– 69% of women have never spoken with a health professional about their pelvic health.
– 1/3 of women do not exercise due to prolapse
– Many women live silently with their symptoms until they become really bothersome
What are the causes of prolapse?
Common risk factors include:
- Pregnancy and childbirth
- Assisted delivery
- Constipation
- Obesity
- Chronic cough
- Excessive or repetitive lifting
What can physiotherapy do to help prevent or treat a prolapse?
Pelvic floor rehab
(down training, strengthening, optimising during function / exercise) 4+ months of pelvic floor exercises under supervision of a professional is the gold standard for prolapse treatment and this can result in an improvement in prolapse position and symptoms.
Modification activity levels
We always try to keep people active and exercising. The benefits of exercise are well known for both physical and mental well being. Stopping exercise for fear of worsening or symptoms is not helpful for any individual or the future progression of a prolapse. Monitoring prolapse position and pelvic floor strength can help to guide an exercise regime that is acceptable to you, it is progressive as your pelvic floor progresses, and gives you the confidence to keep pushing the boundaries beyond what you think is possible.
Treating back injury / stiffness
Stiffness / weakness / injury can contribute to your core stability and prolapse presentation.
Weight management
Any additional weight on top of your organs is going to add pressure to the supporting ligaments and tissues, therefore heading towards a healthy weight is helpful for the future of your prolapse and symptoms from it.
Additional health conditions
Addressing anything that can increase downward pressure on your pelvic floor will help. This can include seeking help for chronic cough or asthma, or speaking with you physiotherapist about ongoing constipation or straining.
Pessary
If you do not see improvement in your symptoms, some ladies will opt for a pessary. A device which sits inside the vagina to support a prolapse and allow improved function with reduced or resolved symptoms.

Need help right now? Book a FEMALE PELVIC HEALTH appointment with JODIE HERE
Jodie our new clinical lead in Pelvic Health brings 18 years of experience of improving the lives of women living with sensitive issues such as pain, prolapse, urinary leakage, bowel leakage and sexual dysfunction. Her experience comes from working as a Clinical Specialist in Female Pelvic Health in the NHS and as clinical educator to Midwives, GP’s, Physiotherapists, Consultants and Registrars in all aspects of pelvic health.